Obsessive-Compulsive Disorder (OCD) and substance abuse are often intertwined, presenting complex challenges for individuals seeking relief. The intense pressures from intrusive thoughts and compulsive behaviors associated with OCD can lead many to turn to substance use as a coping mechanism for persistent anxiety. Unfortunately, this can inadvertently lead to the development of an addiction, compounding an already difficult journey.
The encouraging news is that lasting recovery is genuinely achievable with the right support and a personalized approach to treatment. At Northern Illinois Recovery, we understand that effective healing encompasses the mind, body, and spirit as a unified whole. Our specialized dual diagnosis treatment programs are designed to help individuals manage both OCD and addiction, comprehensively addressing the underlying issues and guiding each person toward a path of lasting well-being.
The typical age of onset for OCD differs, with symptoms often manifesting in childhood. For children, OCD symptoms generally arise between the ages of 10 and 14, with males typically experiencing an earlier onset than females. In adults, the average age of onset is approximately 19 years. Recognizing these symptoms early and understanding OCD are essential first steps in seeking help and finding effective treatment.
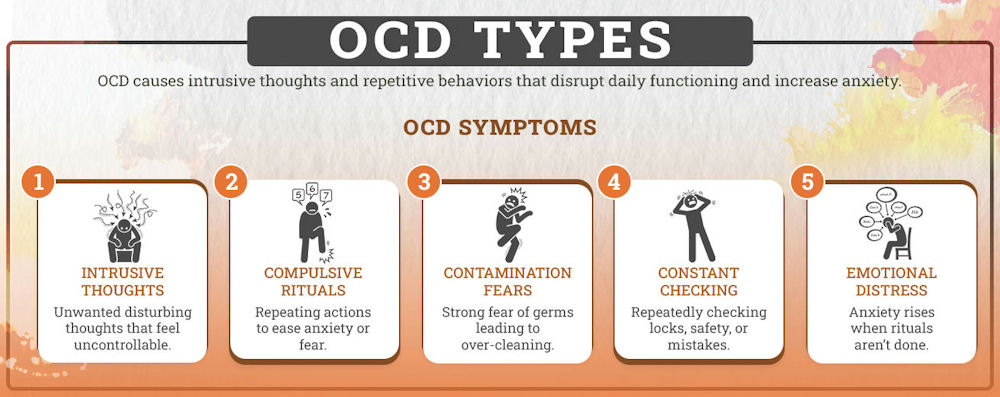
Types of OCD
Individuals with contamination OCD fear exposure to dirt, germs, or any form of contamination. This leads them to engage in excessive cleaning rituals or avoid places they perceive as unhygienic or unsafe, such as public restrooms or certain objects, fearing that contact with them could result in illness or harm.
Individuals with checking OCD feel a compulsion to repeatedly check things like locked doors, turned-off appliances, or light switches. This urge is driven by an intense fear that leaving something unchecked could cause harm, such as a fire or break-in, even though they have already confirmed that everything is secure.
Symmetry OCD involves the need to arrange or align objects in a precise manner. Individuals may experience intense discomfort or anxiety if things are out of place, and the only way to relieve this distress is by arranging items in a way that feels “just right,” even if there is no logical reason for the arrangement.
People with hoarding OCD find it incredibly challenging to discard items, even if they hold no value. This fear stems from the belief that throwing things away could lead to regret or loss, prompting them to accumulate objects, resulting in cluttered living spaces and significant difficulty in organizing or cleaning their environment.
Intrusive thoughts, OCD is characterized by unwanted, disturbing thoughts, often violent, immoral, or sexually inappropriate. These thoughts cause significant distress, and to neutralize the anxiety they provoke, individuals engage in compulsive behaviors or mental rituals, believing that performing these actions will prevent the feared event from occurring.
Prevalence of OCD
The effects of untreated OCD can be profound, impacting not only the individual but also their relationships, work, and daily functioning. Symptoms can result in a diminished quality of life, as individuals often feel overwhelmed by their compulsions and intrusive thoughts. Early diagnosis and treatment are essential for improving outcomes, but many still find it difficult to access the necessary care.
Signs and Symptoms of OCD and Addiction
Common signs of OCD include:
- Fear of contamination or harming others
- Intrusive, violent, or harmful thoughts
- Excessive washing, checking, or repeating actions
- Arranging things in a specific order
- Difficulty stopping rituals despite knowing they are excessive
- Anxiety when rituals are interrupted
Addiction’s signs, on the other hand, include:
- Strong cravings or urges
- Increased tolerance
- Withdrawal symptoms
- Loss of control over behavior
- Continuing despite negative consequences
- Time spent on obtaining, using, or recovering
- Neglecting responsibilities or relationships
- Risky behavior (e.g., driving under the influence)
Addiction vs Compulsion: Is Compulsive Behavior the Same as Addiction?
That said, the two can overlap. Sometimes, people with OCD may resort to substances as a method to cope with their anxiety, leading to what’s called “dual diagnosis.” In these instances, both conditions must be treated together for the best chance of recovery.
OCD and Addiction Treatment
For many men dealing with OCD and substance abuse, stigma presents a significant barrier. Society often pressures men to appear “tough” and in control, making it difficult to open up about their struggles. As a result, they may feel ashamed or embarrassed to admit they need help. This reluctance can lead to underreporting of mental health and addiction issues, which delays the treatment they so desperately need.
Creating a supportive environment where men feel safe to discuss their challenges without fear of judgment is crucial. When they feel understood and not judged, they’re more likely to seek help and begin healing.
For those facing both OCD and substance abuse, a dual diagnosis treatment plan is essential. This approach treats both disorders simultaneously, increasing the chances of long-term recovery. Without this integrated treatment, one condition may exacerbate the other. Typically, dual diagnosis includes therapy, medication, and group support, all designed to help individuals regain control over their lives.
Therapy is central to recovery from both OCD and addiction. For OCD, Cognitive-behavioral therapy (CBT) assists individuals in challenging intrusive thoughts and breaking compulsive behaviors. A specific type of CBT, known as Exposure and Response Prevention (ERP), is particularly effective in helping people confront their fears without reverting to rituals.
In the case of addiction, therapy delves into the emotional and psychological roots of substance use. It includes individual therapy, group therapy, and family therapy sessions, allowing individuals to learn healthy coping mechanisms and begin breaking the cycle of addiction. Therapy is not solely about treatment—it’s about empowering people to rebuild their lives and achieve lasting recovery.
Coping Strategies for OCD and Addiction
Techniques like deep breathing, guided meditation, and body scans help reduce anxiety and manage intrusive thoughts and cravings.
A structured daily routine helps individuals stay focused, reduces uncertainty, and promotes stability, aiding in recovery from both conditions.
Engaging in hobbies, physical activities, or creative outlets can help redirect attention from compulsions or cravings, thereby reducing the risk of relapse.
Regular exercise, a balanced diet, and adequate sleep improve mental health, thereby helping to manage stress in recovery and anxiety that trigger OCD behaviors and substance cravings.
Dual Diagnosis Treatment at Northern Illinois Recovery
Located in serene Crystal Lake, our JAHCO-accredited center is staffed by top-tier addiction treatment professionals, including physicians and licensed clinicians, who utilize evidence-based practices such as cognitive-behavioral therapy and dialectical behavior therapy (DBT). We provide a full continuum of care, from detox and residential to PHP, IOP, outpatient, and aftercare, all focused on achieving outstanding outcomes that exceed industry averages.
Take the courageous first step toward a healthier, more fulfilling life. Contact Northern Illinois Recovery Center today to explore our dual diagnosis programs and begin your path to lasting well-being!